August 07, 2017
The Question: This study, published in Clinical Infectious Diseases, finds evidence that rates of severe methicillin-resistant Staphylococcus aureus (MRSA) blood infections are not declining, despite an overall decline in MRSA-related infections. These findings contradict reported significant reductions in the incidence of invasive MRSA and hospital-onset MRSA bacteremia since 2005 from the U.S. Centers for Disease Control and Prevention (CDC) Active Bacterial Core Surveillance (ABCs) system.
What We Found: Researchers calculated rates of S. aureus and MRSA-related hospitalizations from 2010 to 2014, for septicemias, pneumonias, and unspecified S. aureus infections, using inpatient records from the National Inpatient Survey (NIS) from the Healthcare Cost and Utilization Project of the Agency for Health Research and Quality (AHRQ). The researchers found that hospitalization rates for MRSA-related skin and soft-tissue infections (SSTIs) decreased between 2010 and 2014, while rates for more invasive MRSA-related infections, sepsis, remained constant. The study found:
- The rate of S. aureus septicemias increased nearly 20 percent, from 2.66 to 3.15 per 1,000 hospitalizations. The rate of MRSA septicemias increased from 1.45 to 1.53 per 1,000 hospitalizations and methicillin-susceptible S. aureus (MSSA) septicemia increased from 1.21 to 1.61 per 1,000 hospitalizations.
- MRSA-related skin and soft-tissue infections decreased 29 percent (from 3.8 to 3.0 per 1,000 hospitalizations). The rate of other common primary diagnoses with unspecified MRSA-related infections did not significantly change.
Why It Matters: MRSA is the leading cause of mortality due to antibiotic-resistant infections in the United States. Rates of MRSA remain higher in the United States than most other developed countries, particularly for invasive sepsis and pneumonia, which are often transmitted in hospitals. According to study author and CDDEP Fellow Eili Klein, “It’s important to have an accurate picture of trends in the rates of MRSA infections. That mortality due to sepsis hasn’t declined, despite an overall decline in MRSA infections, underscores the continued need to consider MRSA as a priority in infection control. The overall decrease in Staphylococcus aureus is largely confined to community-associated infections, and may reflect the natural waning of the epidemic.”
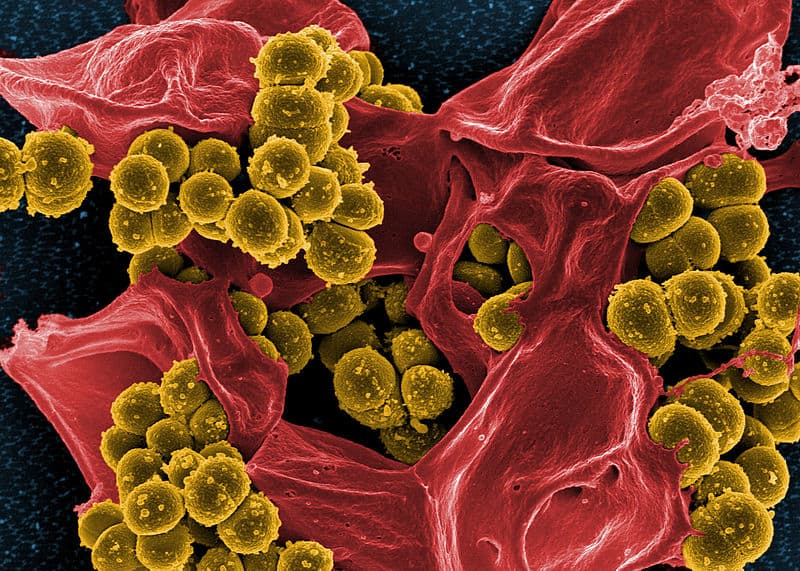
Image via NIAID (CC BY 2.0)

