January 23, 2013
The Question
What is the national epidemiology of Klebsiella pneumoniae isolates resistant to carbapenems (CRKP) and third-generation cephalosporins (G3CRKP)? How do resistance patterns compare across patient care settings, isolate source, geographic region, patient location, and demographic characteristics?
What we found
The proportion of CRKP increased from less than 0.1% to 4.5% between 2002 and 2010. These pathogens, which were endemic only in hospitals in the northeastern United States in the early 2000s, have spread to neighboring regions and are emerging in or being exported to nonacute care settings. The frequency of G3CRKP more than doubled, increasing from 5.3% to 11.5% between 1999 and 2010. G3CRKP and CRKP were more common among elderly patients (those greater than 65 years of age), isolates recovered in the ICU or inpatient setting, and among patients from the northeastern United States. Of note, there was an uptick in the outpatient prevalence of CRKP after 2006, reaching 1.9% of isolates in our sample in 2010.
Why it matters
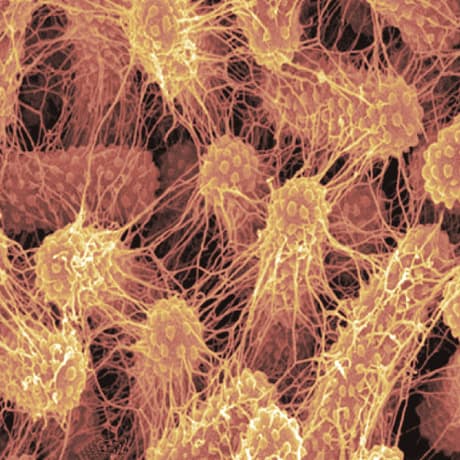
The observed national rise in CRKP is particularly disconcerting for several reasons. First, CRKP infection is associated with a fatal outcome in 47%57% of cases. Second, treatment is limited to older antibiotics known for high kidney toxicitya limitation that highlights the urgent need to develop drugs active against Gram-negative bacteria. Third, the ability of resistance-encoding genes to spread through plasmid transfer enables the spread of resistance to related species like E. coli, a transfer that may occur even in the same patient. Finally, CRKP genes may escape detection in routine laboratory testing. The epidemiology of carbapenem-resistant bacteria thus has the potential to replicate the endemic spread of MRSA beyond hospitals and into the community.

